When Sleep and Pain Collide: The Vicious Cycle of Chronic Pain and Chronic Insomnia
- Lorraine Irlam, Registered Clinical Counsellor

- Sep 14, 2022
- 9 min read
Updated: Feb 1, 2024
Can’t sleep due to chronic pain, or is poor sleep making your pain worse?

Could improving your sleep reduce pain or the need for pain meds?
Chronic pain and chronic insomnia can be among the most debilitating conditions to live with, particularly when they co-occur.
Research found that people with chronic insomnia reported more chronic pain than people without insomnia (50.4% vs. 18.2%).Conversely, individuals with chronic pain reported more chronic insomnia than those without chronic pain (48.6% vs. 17.2%).
I’ve never had an insomnia client with chronic pain who didn’t say their pain is worse after a bad night’s sleep and better after a good one. But the good news is that treating insomnia may be more effective than many realize. And this can go a long way toward improving pain.
Let’s explore the relationship between chronic insomnia and chronic pain and how CBT-I may help alleviate both conditions.
What Is Chronic Pain?
Pain is sensory or emotional discomfort experienced when nerve receptors signal the brain of potential harm. There are two types of pain:
Acute pain is short-term pain from a lesion, disease, or surgery (e.g., cut, fracture, pain after a medical procedure). It resolves as soon as your body has recovered from the issue.
Chronic pain lasts beyond what might be expected, typically more than three months, and is considered a neurological disorder. It can show up in different parts of your body along with an underlying health condition or injury, long after you have otherwise healed, or without an apparent cause.
Common examples of chronic pain include:
Arthritis pain
Back pain
Cancer pain
Headaches and migraines
Muscle, bone, and joint pain (e.g., fibromyalgia)
Post-surgery pain
Temporomandibular pain (TMJ)
Neuralgic pain (i.e., damage to nerves or nervous system),including pain with no apparent physical cause due to central sensitization
Chronic pain may deplete your body, mind, and spirit. It can make working, moving, and living extremely challenging, carrying added mental health issues such as anxiety, depression, and sleep problems.
What Is Chronic Insomnia?
Insomnia consists of problems falling asleep, staying asleep, or getting enough quality sleep despite having the adequate opportunity to do so. There are two categories:
Short-term or acute insomnia typically resolves within a few days or weeks.
Chronic insomnia happens at least three nights a week for more than three months.
Like chronic pain, chronic insomnia can infiltrate many areas of your life and become a vicious cycle. It may involve fatigue, anxiety, depression, difficulty focusing, irritability, and often pain.
The Sleep and Pain Interaction: Does Sleep Affect Pain? Does Pain Affect Sleep?
Chronic pain may disturb sleep.
Many chronic pain patients seek relief by going to bed, yet pain makes sleeping a struggle. Although it’s not a clinical term, some people call this painsomnia. Research indicates that 60% of chronic pain patients attribute insomnia to pain, with 53 to 90% reporting sleep problems happening around or after chronic pain started.
According to a critical review, people experiencing chronic pain may:
Take longer to fall asleep
Have shorter total sleep time
Experience more frequent and prolonged awakenings
Have poorer sleep quality But why does this happen?
Studies state that pain may disturb sleep by triggering arousal and a series of neurobiological processes of stress. This activates an ongoing cycle where disturbed sleep and pain can increase one another. Research shows that pain disrupts sleep, while sleep loss can result in an increase in pain intensity, flare-ups, and a 2.5-fold increased risk of new onset chronic pain.
Sleep disruptions may contribute to chronic pain.
When you sleep, you go through various phases: falling asleep, light sleep, slow-wave sleep (SWS), and rapid eye movement (REM). Poor quality and disrupted sleep may rob you of any of these stages, raising the risk of new chronic pain, worsening existing chronic pain, and influencing pain fluctuations.
While all stages of sleep are important for various functions, SWS is the deep, restorative sleep phase, critical for cellular, muscle, and tissue repair, and for supporting your development and immune function.
SWS helps regulate pain systems. Lack of SWS can interrupt your body’s natural ability to inhibit pain and cause increased pain sensitivity. Evidence shows that disrupted SWS may also be associated with reduced pain threshold, increased discomfort, fatigue, and inflammatory flare-ups.

Other conditions can also fuel the vicious cycle.
If you struggle with chronic pain and/or chronic insomnia, not surprisingly, you may also grapple with depression, anxiety, stress, and fatigue. All of these challenges can exacerbate insomnia and impact your pain regulation systems.
Now, if you experience insomnia and pain in the context of other conditions such as a traumatic brain injury (TBI) or multiple sclerosis (MS), the journey might be even more challenging. Your symptoms can feed pain and insomnia, so coping might seem like a lost battle. For example, while exercise can help with sleep and depression, people struggling with chronic pain from MS might find it too demanding. This can impact motivation and your ability to push through, causing more sleep loss and hopelessness.
In addition, many of the coping mechanisms chronic pain patients resort to (e.g., pain medications, lying awake in bed) can unknowingly fuel chronic insomnia and exacerbate pain.
In any case, difficulty coping with a chronic condition can add to the seemingly hopeless spiral.
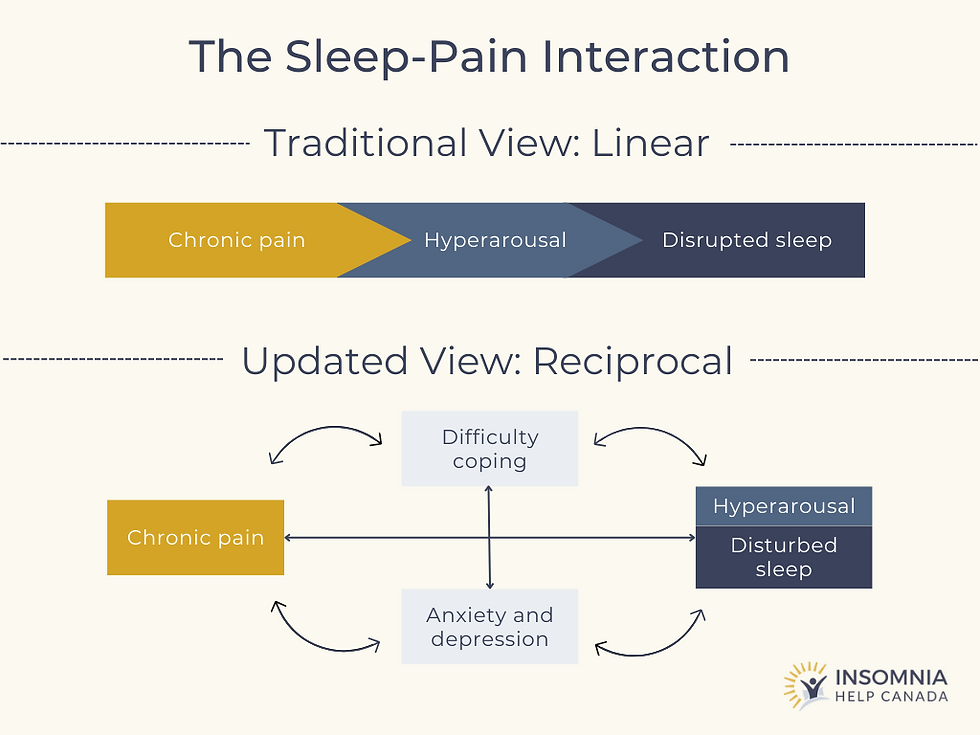
Challenging the linear connection between pain and sleep.
Traditionally, it was believed that pain itself caused sleep disturbances. And while that’s certainly true, you can see that it’s more complex than that.
The above findings challenge the linear connection between pain and sleep. Recent theories show a reciprocal relationship where pain, sleep disruption, anxiety, depression, and difficulty coping all interact to fuel a vicious cycle of impaired pain inhibition capacity, increased central sensitization, and insomnia.
Could improving sleep reduce the need for opioids and other medications?
One of the main challenges of chronic pain treatment is the lack of safe, long-term options. Many people suffering from debilitating pain resort to prescription opioids, desperately longing for relief.
However, research shows opioids can stimulate the nervous system and make it “abnormally sensitized” to pain. Further evidence indicates that acute use of opioids may result in decreased REM sleep and slow-wave sleep, as well as increased wakefulness and sleep fragmentation. A recent randomized trial also stated that multiple awakenings might reduce opioids’ analgesic effects. In summary, opioids may increase pain sensitivity, disrupt sleep, and become less effective with increased awakenings, feeding the reciprocal pain-sleep spiral. Another fascinating study found that caffeine reduced pain sensitivity in sleep-deprived mice but not in rested mice. It noted that “pain may be reduced not by analgesics, whose effectiveness is reduced, but by increasing alertness or providing better sleep.” The implication of all this is that sleep deprivation may lead to an increased need for pain meds.
Given the opioid crisis, organizations like the CDC offer prescribing guidelines to make opioid use safer (if necessary). These policies highlight that nonopioid therapy is preferred for chronic pain and that providers should only consider opioids if the benefits for pain and function outweigh the risks.
One of those nonopioid therapy options Cognitive behavioural therapy for insomnia (CBT-I)(Please note: this is not the same as CBT for chronic pain).
CBT for insomnia (CBT-I) may reduce pain.
Cognitive behavioural therapy for insomnia (CBT-I) is the first line of treatment for chronic insomnia. It’s an evidence-based and drug-free approach as effective as sleep medications within a few weeks but safer and longer lasting.
CBT-I offers practical strategies to address what’s disrupting your sleep regulation systems. It helps consolidate sleep, improving sleep time and sleep quality—specifically SWS. And while it may not cure chronic pain conditions, it typically allows people to sleep longer through the pain and return to sleep more quickly after being awakened by pain.
CBT-I has been called a “gateway treatment.” For example, it frequently reduces depression and anxiety, in addition to insomnia. People living with chronic pain may benefit from CBT-I to get better sleep and potentially decrease the need for pain medication.
For instance, a sleep medicine study showed significant improvements in pain interference with daily functioning after eight weeks of CBT-I. And a recent systematic review found the probability of having less pain after CBT-I to be 58% (post-treatment) and 57% (after up to 12 months).
While this gold standard insomnia therapy may need some modification for chronic pain patients, it can often help break down the vicious loop between insomnia and pain. For example, lying in bed too long can actually condition the body to associate the bed with insomnia, instead of sleep. It’s called “conditioned arousal” and tends to fuel worse insomnia in the long run. Ever feel exhausted all day, but as soon as bedtime nears, tiredness becomes “tired, but wired”? That’s likely conditioned arousal at play. But people with chronic pain often need to lie down and rest. So, then what? Here are a few harm reduction strategies:
When possible, lie in a different room, a different bed, a couch during the day – or when you can’t sleep at night
If that’s not an option, sit up in bed, or arrange your comfy pillows (preferably different pillows) in a different position than you use at night
Lie on the opposite side of the bed
Lie on top of the covers, instead of between the sheets
Lie on top of a different coloured blanket
Wear daytime clothes, instead of sleepwear
Use different lighting during the day
Keep the blinds open
Anything that creates a different ambience can be surprisingly helpful to avoid further training the body to have insomnia in bed at night.
Why not give CBT-I a shot? Worst-case scenario—you learn how to improve your sleep. Best-case scenario—you help alleviate your pain. Improved pain can be a welcome side effect for many!

Need Support?
Always consult with your physician about the best treatment for your pain.
If you are struggling with chronic pain and chronic insomnia and believe that better sleep may relieve your pain, we are here for you.
Insomnia Help Canada offers CBT-I services throughout much of Canada and a self-paced online program available worldwide to help you reclaim your life with better sleep.
We know it’s been a long ride, but there is hope. If you’re interested in one-on-one sessions, contact us for a free consultation.
References:
1. Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care. 2016
Oct-Dec;5(4):780-784. doi: 10.4103/2249-4863.201153. PMID: 28348990; PMCID:
PMC5353813. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5353813/
2. Loeser JD, Melzack R. Pain: an overview. Lancet. 1999 May 8;353(9164):1607-9. doi: 10.1016/S0140-6736(99)01311-2. PMID: 10334273.
https://pubmed.ncbi.nlm.nih.gov/10334273/
3. Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009 Sep;10(9):895-926. doi: 10.1016/j.jpain.2009.06.012. PMID: 19712899; PMCID: PMC2750819.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2750819/
4. Summer, J. Painsomnia. Sleep Foundation. 2022, June 17. https://www.sleepfoundation.org/physical-health/painsomnia
5. Tang NK. Insomnia Co-Occurring with Chronic Pain: Clinical Features, Interaction, Assessments and Possible Interventions. Rev Pain. 2008 Sep;2(1):2-7. doi: 10.1177/204946370800200102. PMID: 26525182; PMCID: PMC4589931. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4589931/ 6. Bjurstrom MF, Irwin MR. Polysomnographic characteristics in nonmalignant chronic pain populations: A review of controlled studies. Sleep Med Rev. 2016 Apr;26:74-86. doi: 10.1016/j.smrv.2015.03.004. Epub 2015 Apr 8. PMID: 26140866; PMCID: PMC4598249. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4598249/ 7. B Kundermann, J-C Krieg, W Schreiber, S Lautenbacher. The effect of sleep deprivation on pain. Pain Res Manage 2004;9(1):25-32.
8. Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013 Dec;14(12):1539-52. doi: 10.1016/j.jpain.2013.08.007. PMID: 24290442; PMCID: PMC4046588.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4046588/
9. Lentz MJ, Landis CA, Rothermel J, Shaver JL. Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women. J Rheumatol. 1999 Jul;26(7):1586-92. PMID: 10405949.
https://pubmed.ncbi.nlm.nih.gov/10405949/
10. Lind J, Andréll P, Grimby-Ekman A. Insomnia Symptoms and Chronic Pain among Patients Participating in a Pain Rehabilitation Program - A Registry Study. J Clin Med. 2021 Sep 7;10(18):4040. doi: 10.3390/jcm10184040. PMID: 34575149; PMCID:
PMC8468051. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8468051/
11. Centers for Disease Control and Prevention. Prescription Opioids. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. 2017, August 29. https://www.cdc.gov/opioids/basics/prescribed.html
12. Tracy, J. Opioid-induced Hyperalgesia. Institute of Chronic Pain. 2014, April 25. https://instituteforchronicpain.org/understanding-chronic-pain/complications/opioid-induced-hyperalgesia
13. Angarita, G.A., Emadi, N., Hodges, S. et al. Sleep abnormalities associated with alcohol, cannabis, cocaine, and opiate use: a comprehensive review. Addict Sci Clin Pract 11, 9 (2016). https://doi.org/10.1186/s13722-016-0056-7
14. Robertson JA, Purple RJ, Cole P, Zaiwalla Z, Wulff K, Pattinson KTS. Sleep disturbance in patients taking opioid medication for chronic back pain. Anaesthesia. (2016) 71:1296–307. doi: 10.1111/anae.13601.
https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/full/10.1111/ anae.13601
15. Smith, M.T.,Mun, C.J., Remeniuk, B. et al. Experimental sleep disruption attenuates morphine analgesia: findings from a randomized trial and implications for the opioid abuse epidemic. Sci Rep 10, 20121 (2020).
https://doi.org/10.1038/s41598-020-76934-1
16. Alexandre C, Latremoliere A, Ferreira A, Miracca G, Yamamoto M, Scammell TE, Woolf CJ. Decreased alertness due to sleep loss increases pain sensitivity in mice. Nat Med. 2017 Jun;23(6):768-774. doi: 10.1038/nm.4329. Epub 2017 May 8. PMID: 28481358; PMCID: PMC5798598.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5798598/
17. Centers for Disease Control and Prevention. Understanding the Epidemic. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. 2021, March 17. https://www.cdc.gov/drugoverdose/epidemic/index.html
18. Centers for Disease Control and Prevention. About CDC’s Opioid Prescribing Guideline. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. 2022, August 16. https://www.cdc.gov/opioids/providers/prescribing/guideline.html
19. Carla R. Jungquist, Chris O’Brien, Sara Matteson-Rusby, Michael T. Smith, Wilfred R. Pigeon, Yinglin Xia, Naiji Lu, Michael L. Perlis, The efficacy of cognitive-behavioral therapy for insomnia in patients with chronic pain, Sleep Medicine, Volume 11, Issue 3, 2010, Pages 302-309, ISSN 1389-9457.
20. Janannii Selvanathan, Chi Pham, Mahesh Nagappa, Philip W.H. Peng, Marina Englesakis, Colin A. Espie, Charles M. Morin, Frances Chung, Cognitive behavioral therapy for insomnia in patients with chronic pain – A systematic review and meta-analysis of randomized controlled trials, Sleep Medicine Reviews, Volume 60, 2021, 101460, ISSN 1087-0792. https://doi.org/10.1016/j.smrv.2021.101460
21. Monica Haack, Understanding Sleep Problems and Long Covid. National Institue of Health. 2023 September 12. https://covid19.nih.gov/news-and-stories/understanding-sleep-problems-long-covid


Comments